Page History
...
- Click the Patients tab.
- Click Patient Search/Add in the left hand navigation bar, and then search for the patient.
- Select the patient from the search results.
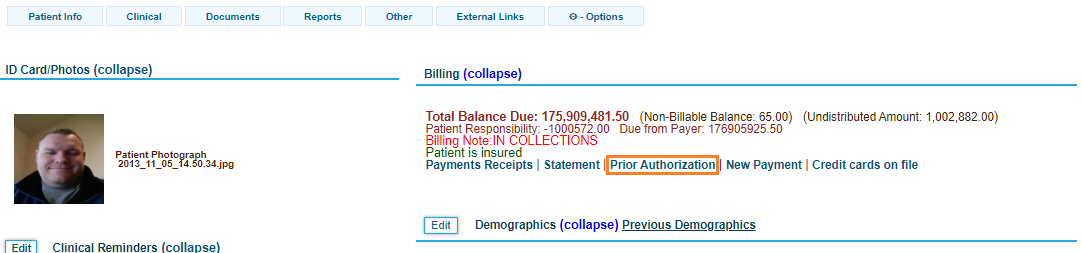
The Patient Summary Chart page opens. - Click the Prior Authorization link below the Billing header.
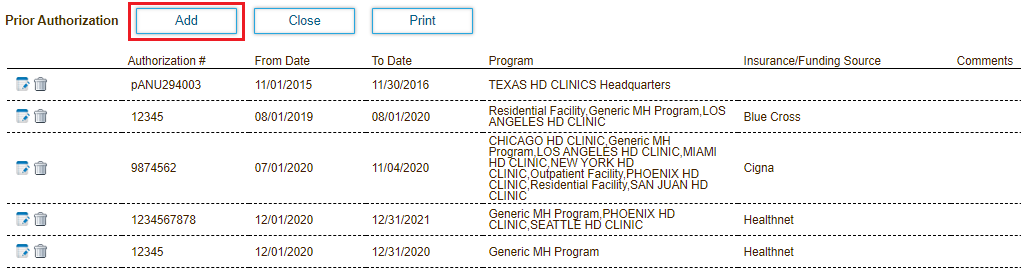
- Click the Add button to open the Add Prior Authorization popup window.
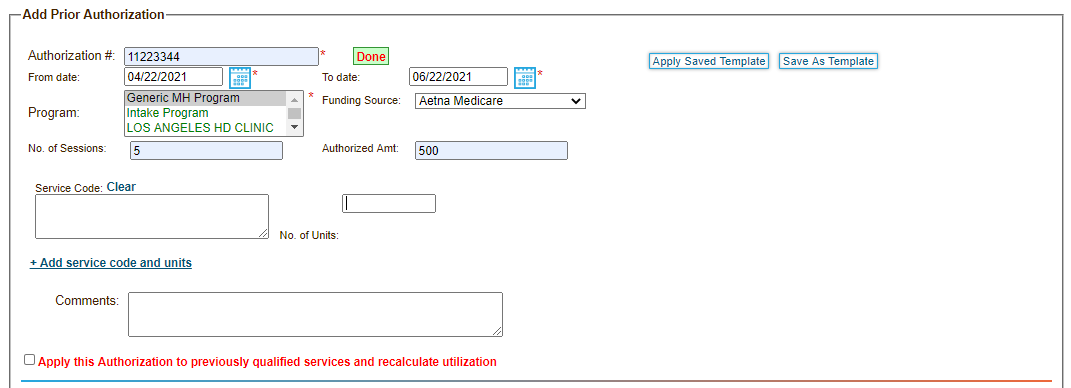
- Enter the prior authorization number (PAN) provided by the insurance company in the Authorization # field. The application alerts you if the number already exists in the system.
- Enter the "From" and "To" dates the authorization is valid for.
- Select the facility authorized to provide services.
- Select the Insurance company providing the authorization.
- Enter the number of approved sessions.
Each session is equal to one day. Multiple encounters that occur in a single day are considered to be one session. - Enter the total billable amount the insurance company is willing to pay for the services provided.
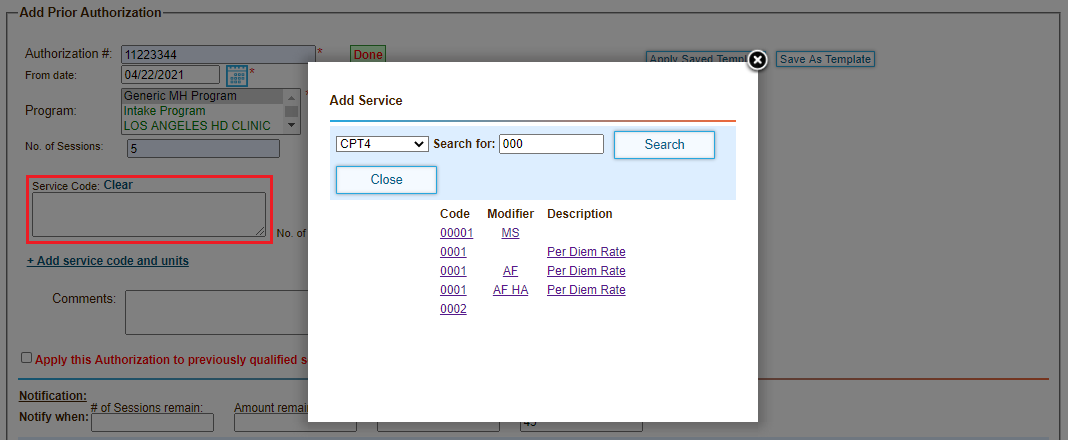
- Click in the Service Codes field. The Add Service dialog opens.
- Search for and add the service code and modifier for each authorized services to be provided.
- Add the number of units approved for each service code.
- Specify when to alert the provider to ensure the services provided align with what the insurance company is willing to cover. Notifications can be sent based on the following thresholds:
- The number of remaining authorized sessions
- The authorized billable amount balance
- The number of remaining authorized billable service units
- The number of days before the prior authorization number (PAN) expires
- Check Inbox, Email or both to indicate how notifications are sent to the provider delivering services.
- Click Save.
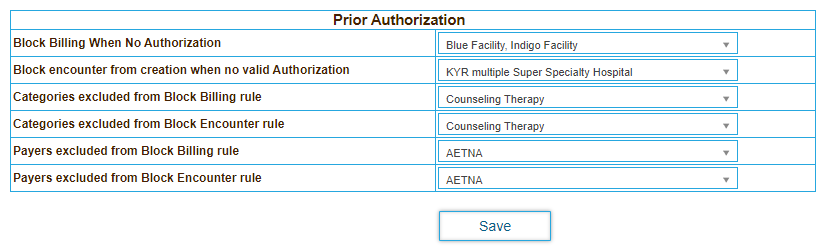
Block Billing or Encounters for Facilities if Patients Do Not Have Prior Authorization
...
- Click the Practice tab.
- Expand Feature Settings in the left menu bar, and then expand Billing.
- Click Prior Authorization.
- Select the facilities to apply the billing or encounter creation rules to.
- Optionally select the categories or payers to exclude from the selected rules.
- Click Save.
...
Overview
Content Tools
Activity